The National Medical Commission, NMC has released the Guidelines For Competency-Based Postgraduate Training Programme For DM In Geriatric Mental Health.
The Principles adopted by UN General Assembly resolution 46/119 of 17 December for the protection of persons with mental illness and the improvement of mental health care (MI Principles) recognise the enjoyment of the highest attainable standard of physical and mental health as the right of every human being. This resolution should now be read in the context of the United Nations Convention on the Rights of Persons with Disabilities. In 1996, WHO developed the Mental Health Care Law: Ten Basic Principles as a further interpretation of the MI Principles and as a guide to assist countries in developing appropriate legislation on mental health. The WHO also developed Guidelines for the Promotion of Human Rights of Persons with Mental Disorders.
The principles governing the treatment of persons with mental illness can be summarized as follows:
• The aim of psychiatry is to treat mental illness and promote health to the best of his/her (psychiatrist’s) ability, consistent with accepted scientific knowledge and ethical principles;
• Every psychiatrist should offer to the patient the best available therapy to the best of his/her knowledge;
• The psychiatrist should inform the patient of the nature of the illness, therapeutic procedures including possible alternatives and of the possible outcome;
• No procedure shall be performed nor treatment given against or independent of a patient’s own will, unless because of mental illness, the patient cannot form a judgment as to what is in his/her best interest and without which treatment serious impairment is likely to occur to the health of the patient or others;
• As soon as the conditions for compulsory treatment no longer apply, the psychiatrist should release the patient from the compulsory nature of the treatment and if further therapy is necessary should obtain voluntary consent;
• The value of positive mental health for every human being and the rights of all persons with mental disorders and with disabilities as full citizens of their countries should be recognized;
• All recipients of mental health services, regardless of age, gender, ethnic group or disorder must be treated in the same manner as other citizens in need of health care and their basic human rights and freedoms should be respected.
At the end of the DM training program, the post graduate student should be able to recognize the health needs of the community, should be competent to handle effectively psychiatric problems and should be aware of the recent advances in Psychiatry. He /she should acquire necessary skills in teaching medical / paramedical students. He / she is also expected to know the principles of research methodology.
National Goal: This document aims to provide broad Guidelines to orient post graduate students of Psychiatry and Geriatric Medicine on the importance of appropriate geriatric mental health care, familiarize them to the mental and other specific problems of the elderly, inculcate in them competencies on mental health care of the elderly and expose them to legal and ethical issues.
Eligibility requirements:
MD (Psychiatry), MD (Geriatrics /Geriatric Medicine)
SUBJECT SPECIFIC OBJECTIVES
Theoretical Knowledge: The primary goal of the program is to train post graduate DM students in the treatment and management of geriatric mental health patients. To achieve this goal, the student should:
1. Discuss and define the importance of the geriatric mental health in the context of the health needs of the community and the national priorities in the health sector.
2. Acquire in-depth understanding of the basic sciences relevant to the practice of Geriatric Mental Health.
3. Identify social, economic, environmental, biological and psychological determinants of health in the geriatric population, and take these into consideration
while planning preventive, therapeutic, rehabilitative, and promotive measures/strategies.
4. Acquire knowledge and skills for educating medical and paramedical professionals in geriatric mental health care.
5. Demonstrate appropriate behavior while dealing with the mental health needs of the geriatric subjects and their families, in alignment with the principles of the National Health Policy.
6. Participate in various components of National Mental Health Program.
Practical and Clinical skills: The DM program in Geriatric Mental Health is devoted principally for clinical training, involving both inpatient and outpatient activities. The post graduate students should therefore achieve adequate skills, always undertake ethical and evidence-based practice for prevention of mental ill-health, and also for the diagnosis, management and rehabilitation of elderly patients with mental health problems.
Attitudes including communication skills: The post graduate student should acquire adequate communication skills for dealing with mentally ill patients, their relatives and attendants. Regular clinical rounds and academic presentations during the teaching program should help the trainees to develop patient-appropriate attitude, knowledge and communication skills.
Training in Research Methodology: In-house training in research methodology, Ethics and Biostatistics should be encouraged by requiring to attend workshops/courses.
SUBJECT SPECIFIC COMPETENCIES
At the end of the course, the student should be able to acquire the following competencies under the three domains, viz., cognitive, affective and psychomotor:
Cognitive domain (Knowledge domain)
By the end of the course, the post graduate student should develop the following competencies through hands-on learning while working with the geriatric population with mental health problems: To achieve this, the student should:
- Be able to prepare detailed history of the patient with geriatric mental health disorders in order to be able to diagnose correctly the clinical condition, order appropriate investigations and advise the treatment plan.
- Acquire theoretical competencies that would help to provide comprehensive psychiatric medical care which is compassionate, appropriate, and effective for the treatment of mental health problems and for the promotion of improved mental health of older adults suffering from psychiatric and neuropsychiatric disorders.
- o Acquire knowledge regarding management of various ethical and legal issues related to mental health of the geriatric patient such as:
– assessment of decisional capacity,
– palliative care including legislative guidelines governing prescribing psychotropic substances in nursing home,
– guardianship,
– ethical issues including right to refuse treatment,
– refusal to undergo medical treatments,
– end-of-life issues.
aggressiveness, wandering, changes in sleep patterns, incontinence, aggressiveness) strategies, including physical restraints and their limitations.
- Acquire knowledge regarding legislative guidelines governing psychotropic- prescribing in nursing home/s.
- Identify geriatric patients with problems that are likely to be appropriate for various psychotherapies (e.g., interpersonal therapy (IPT), cognitive behavioral therapy (CBT), problem-solving therapy (PST), dynamic therapy, and reminiscence therapy).
- Acquire knowledge on the principles and indications for use of electroconvulsive therapy (ECT) in the elderly.
- Acquire knowledge regarding the interaction of neuro-pharmacological agents used in geriatric patient care with other medications in use and be able to provide appropriate advice.
- Practice evidence-based medicine: make informed decisions about therapeutic interventions that are based on patient evaluation/preferences, scientific data and clinical judgment.
- Describe and discuss the hazards which geriatric mentally ill patient may encounter in hospital and protection in terms of psychological hazard.
- Ensure quality assurance of investigations and therapeutic procedures.
- Discuss the concept of essential drugs and their rational use with particular emphasis on use in geriatric patients with mental health issues.
- Demonstrate the ability to organize psychiatric assistance to public during disasters resulting in mass casualties.
- Demonstrate the ability to organize psychiatric assistance to public during pandemics resulting in mass casualties.
- Describe the physical and chemical restraints used in emergency psychiatric situations (e.g., violence, delirium etc.)
- Develop a psychiatric geriatric unit and drug dependence treatment unit with essential equipment.
- Describe and discuss legal issues in the practice of geriatric Psychiatry.
- Discuss the application of Clinical Psychology as related to geriatric Psychiatry.
- Discuss the modalities for rehabilitation of geriatric psychiatry patients.
- Describe and discuss community geriatric psychiatry
- Describe and discuss geriatric sexuality and sleep disorders.
- Interact with faculty and teams from other disciplines including General Medicine, Family Medicine, Neurology and Physical Medicine and Rehabilitation.
Affective domain (Attitudes including Communication and Professionalism)
The DM candidate at the end of training should demonstrate the ability to:
• Be able to communicate in a professional manner the treatment plan with patients, their family and care givers,
• Be able to function as a part of a team in collaboration with other geriatric mental health care team members including those from related clinical disciplines, psychiatric nursing/occupational therapy staff and nutrition unit.
• adopt ethical principles and maintain proper etiquette in dealing with patients, relatives and other health personnel and to respect the rights of the patient including the right to information and second opinion.
• develop communication skills to word reports and professional opinion and to interact with patients, relatives, peers and paramedical staff, and for effective teaching.
Leadership skills
• organize team activities in the department and community on geriatric mental health care.
• plan and implement group activities with health staff in the hospital and community.
Professionalism
• Accepts personal responsibility for care of patients with mental health problems, consistent with good work ethics and empathy.
• Demonstrates appropriate truthfulness and honesty with colleagues.
• Recognizes personal beliefs, prejudices, and limitations, which should not come in the way of providing service.
• Respects patient confidentiality at all times in verbal and written communication.
Attitude
• Respects patients’ religious, moral, and ethical beliefs and biases, even if they differ from the student’s own beliefs.
• Presents all available options accurately and non-directively to the patient and relatives.
• Is aware of the advantages and potential hazards of referring patients and families to community or to national resources.
• Recognizes the limitations of their own skills and seeks consultation when necessary.
• Demonstrates understanding of and sensitivity to end-of-life care and issues regarding provision of care.
Interpersonal and Communication Skills Human Relationships
• Demonstrates an effective system for identifying and addressing ethical, cultural, and spiritual issues associated with health care delivery to geriatric mental health patients.
• Demonstrates knowledge or applies an understanding of psychological, social, and economic factors which are pertinent to the delivery of health care to geriatric mental health patients.
• Effectively engages the patient and/or family in communications which are non- judgmental and non-coercive.
Psychomotor Domain (subject specific practice based or practical competencies)
a) By the end of the course, the DM student should be able to perform independently, the following procedures:
• Obtain essential and accurate information, through interviews, with geriatric psychiatric patients, family members, caregivers and other health professionals, with attention to:
• relevant patient history including direct or indirect abuse of the elderly,
• examination of mental status of patient including structured cognitive assessment,
• Mental Status Examination including Instrumental Activities of Daily Living (IADL), Activities of Daily Living (ADL), frailty and different frailty index and sarcopenia,
• assessment of capacity to take decisions regarding treatment, personal care etc,
• medical evaluation including detailed neurological examination, changes in sleep pattern and aggressiveness,
• Clinical IQ / cognitive assessment,
• Assessment of extent of family support,
• availability of efficient and compassionate care giver,
• community support and safety issues.
• Order appropriate laboratory investigations to help in diagnostic evaluation.
• Diagnose common psychiatric illnesses after clinical examination and on the basis of results of laboratory investigations.
• Develop protocol for a comprehensive treatment plan which would address biological, psychological, and sociocultural domains.
• Prepare a comprehensive case record with all relevant information.
• Obtain proper informed consent.
• Perform on basis of appropriate indications electroconvulsive therapy (ECT) in the elderly.
• Make informed decisions about therapeutic interventions based on patientinformation and preferences, up-to-date scientific evidence in the field, and clinical judgment.
• Perform neuropsychological assessment in geriatric setting.
• Perform Medical audit, as per established protocol.
• Prepare a detailed discharge summary with all relevant information.
b) The DM student should be able to perform under supervision, the following procedures:
- Behavior therapy: behavioral treatment specially in dementia patients, using non-pharmacologic approaches, knowing the limitations of behavioral therapeutic strategies, including physical restraints.
- Psychotherapy: identify patients with problems suitable for the various psychotherapies (e.g., interpersonal therapy (IPT), cognitive behavioral therapy (CBT), problem-solving therapy (PST), dynamic therapy, and reminiscence therapy).
- Management of various types of substance abuse as well as withdrawal management.
- Management of acute drug toxicity like Neuroleptic malignant syndrome (NMS), Acute dystonia etc.
- Genetic Counseling and Family therapy
- The management of patients with suicidal tendencies/ attempt at suicide.
c) The student, at the end of the course should be able to assist in the following:
• Interpersonal therapy
• rTMS (Repetitive transcranial magnetic stimulation) therapy
• TDCS (Transcranial Direct-Current Stimulation) therapy
Syllabus
Course contents:
The student should acquire knowledge in the following areas:
First Year
A: The Basic Sciences as applied to Geriatric Mental Health I: The Myth, History, Science and Theories of aging:
• The prolongation of youth and life
• Attitudes towards aging
• Definition of aging
• Biological theories of aging:
• Psychological theories of aging
• Social theories of aging
• Length of life: the sex differential
• Stem cells and aging
II: Neuroanatomy, Neurophysiology, Neuropathology and Neuropharmacology of Aging and Behaviour:
• Neuroanatomy:
- Brain development
- Neuroanatomy and aging brain
• Brain stem
• Prosencephalon
• Cerebral cortex and its connections
• Association cortex
• Organisation of sensory-motor systems
• Limbic system
• Neurophysiology:
- Electrophysiological studies in the psychiatric evaluation of the elderly
• Electroencephalogram (EEG)
• EEG changes with normal aging, dementia, delirium, depression
• Magneto Encephalography (MEG)
• Neuropathology:
- Normal aging
- Alzheimer’s disease
- Dementia with Lewy bodies or vascular dementia
- Frontotemporal dementia
• Neuropharmacology of behaviour:
- Neural transmission of information
- Principles of chemical neurotransmission
- Receptors, enzymes and chemical neurotransmission as the target of drug action
- Special properties of receptors
- Biogenic Amines and behavioral functions:
• Norepinephrine
• Dopamine
• Serotonin
• Histamine
- Acetylcholine and behavioral functions
- Non-neuropeptides and behavioral functions
• Prostaglandins
• Thromboxanes
• Purines
- Neuropeptides and behavioral functions:
• Endogenous Opioids
• Gut peptides
• Hypothalamic, Pituitary and Pineal peptides
III: Genetics of Geriatric Psychopathology:
• Fundamentals of Genetics: o Molecular Genetics
- Linkage analysis
- Candidate gene
• Genetic factors in normal and accelerated aging:
- Cognitive impairment with advancing aging
- Cellular aging research
• Methodology in psychiatric genetics:
O Traditional methods
- Pedigree and family studies
- Twin studies
- Adaptation studies
• Interpretation of genetic results.
• Genetics of Psychiatric disorders of old age: o Cognitive and motor disorders:
• Alzheimer ‘s disease
• Multi-infarct dementia
• Parkinson’s disease
• Huntington’s disease
• Pick’s disease
• Transmissible dementias
• Creutzfeldt-Jacob disease
• Gerstmann-Straussler-Scheinker Disease o Non-Cognitive disorders:
• Schizophrenia and related psychosis
• Mood disorders
• Schizo-affective disorder
• Anxiety disorders
• Adjustment disorders
• Sleep disorders
• Sexual disorders
• Alcohol and substance abuse disorders
IV: Physiological and Medical considerations of Geriatric Patient Care:
• Central Nervous system
• Cardiovascular system
• Respiratory system
• Gastrointestinal system
• Endocrine system
• Musculoskeletal system
• Haematological and immune systems
• Renal system
• Considerations in geriatric prescribing
• Chronic diseases in elderly
• Geriatric syndromes
• Geriatric assessment
V: Psychological Aspects of Normal Aging:
• Experimental and cognitive psychology
• Neuroimaging and neurosciences
• Behavioural medicine and health and behaviour relationships
• Health and disease interaction with intellectual and cognitive functioning
• Health and self-related health
• Personality and aging in the social context
• Coping in later life
• Care-giving issues in the normal psychology of aging
• Longevity and the extreme aged
VI: Social and economic factors related to Psychiatric Disorders in late life:
• Social risk factors for psychiatric disorders
• Age changes and cohort differences in social risk factors
• Social factors that affect recovery from psychiatric disorders
• Help seeking for psychiatric disorders
• Public policies and programs
VII: Demography and Epidemiology of Psychiatric disorders in late life:
• Demography
• Case identification
• Distribution of psychiatric disorders
• Historical studies
• Etiological studies
• Health service utilization
VIII: Human Development through Life Cycle:
• Infant development
• Childhood development
• Adolescent development
• Adult development
• Normal aging – psychological, socio-cultural, physiological aspects
• Self experience across the second half of the life
IX: Contribution of Intra-psychic and phenomenological theories in Psychopathology of late life:
• Intrapsychic theories
- Freudian approach
- Jungian approach
- Adlerian approach
- Interpersonal and social approaches
- Ego theories
• Phenomenological theories
- Existential movement
- Humanistic movement
- Behavioural theories
- Classical and Operant conditioning theories
- Drive reduction and reciprocal inhibition theories
- Social learning and other psychobiological approaches
SECOND YEAR
Principles and Practice of applied sciences (clinical) in Geriatric Mental Health
I: The History and diagnostic interview in late life:
• The Psychiatric interview of older adults:
- History
- Physical examination
- The mental status examination
- Family assessment
- Rating scales and standardized interviews
- Effective communication with the older adults
• Use of the Laboratory in the diagnostic workups: o Complete blood count
- Serological tests for syphilis
- HIV testing
- Thyroid Function Test
- Vit-B12, Folate and homocysteine
- Toxicology
- Urine analysis
- ECG, EEG, Polysomnography
- Imaging Studies: CT Scan, MRI
- Genetic testing, Apo-E testing
- Ethical and psychological concerns
• Neuropsychological Assessments:
- Neuropsychological assessment in geriatric settings
- Neuropsychology of normal aging
- Differentiation of Alzheimer’s Dementia from normal aging
- Neuropsychological profile of following disorders:
• Mild cognitive impairment
• Alzheimer’s disease
• Frontotemporal dementia
• Lewy body dementia
• Vascular dementia
• Parkinson’s disease dementia
• Huntington ‘s disease
• Progressive Supranuclear Palsy
• Hydrocephalus
• Creutzfeldt-Jakob disease
• Dementia of geriatric depression
• Stroke
• Motor neuron disease
• Demyelinating disorders
II: Clinical Phenomenology and Psychopathology in late Life:
• Disorders in general appearance and behavior
• Disorders of consciousness and orientation
• Disorders of attention and concentration
• Disorders of affect
• Disorders of thinking
• Disorders of perception
• Disorders of memory
• Disorders of intelligence
• Disorders of insight and judgment
III: Socio-cultural foundations of behavior related to late life:
• Normality and Abnormality:
- Concept of mental health and illness
- Attitudes towards mental illness, stigma and social identity
- Epidemiological studies and socio-demographic correlates of mental illness in India.
• Family:
- Personality formation in the family: parent child Dyad
- Early development and communication pattern: triadic relationship, family norm
- Self-image and self-esteem
- Impact of mental illness on the family: the attribute of responsibility, decision taking, role performance, Power Orientation, care giver burden.
- Problems due to family, society, community and generation gap in old age.
• Disturbance in Interpersonal Processes:
- Personal relationships in different mental disorders of old age.
- Abnormal self-attitudes, self -perceptions, self-other perceptions, social competence, interpersonal perceptions.
• Socio-psychological Methods:
- Clinical applications of social identity, interdependence, social skill and interaction models.
• Trans-cultural Aspects:
- Socio-cultural studies of socialization: culture and mental illness, social class and mental illness, religion and mental illness, social change.
- Ancient Indian concepts of mind: cognition, emotion, motivation, stress, personality and their relevance to modern health.
• Concepts of mental illnesses and its treatment in ancient Indian thought, and promotive aspects of mental health
• Contemporary Indian concepts, theories and models used in geriatric mental health.
IV: Neuropsychology in late life:
• Frontal Lobe Syndrome:
- Basic Anatomy
- Pre-frontal Cortex
- Disturbance of regulatory functions
- Disturbance of attentional processes
- Disturbances in emotion, memory and intellectual activity
- Premotor Cortex: disturbances in psychomotor functions
• Temporal Lobes Syndrome:
- Basic Anatomy
- Special senses, hearing, vestibular functions
- Integrative functions
- Disturbances in learning and memory functions
- Disturbances in speech
- Disturbances in emotions, time perception and consciousness
• Partial and Occipital Lobes Syndrome:
- Basis Anatomy
- Disturbances in sensory functions and body scheme perception
- Agnosias and Apraxias
- Disturbances in visual space perception
- Disturbances in visual memory
- Disturbances in emotions, time perception and consciousness
• Functional specialization of Cerebral Hemisphere
- Handedness and cerebral dominance
- Split brain and reported studies on cerebral lateralization of functions.
- Plasticity and restoration of functions.
• Psychophysiology
- Methodology and measurement.
- Psychophysiology of cognition and emotional states
- Studies in psychiatric conditions
III: Psychiatric Disorders in Late Life:
• Cognitive disorders
• Movement disorders
• Mood disorders
• Schizophrenia and paranoid disorders and other psychosis
• Anxiety and panic disorders
• Somatoform disorders
• Sexual disorders
• Bereavement and adjustment disorders
• Sleep and circadian rhythm
• Alcohol and drugs associated problems
• Personality disorders
• Agitation and suspiciousness
• Sub-syndromal mental health problems
IV: Treatment of Psychiatric Disorders in late life:
• Principles and practice of:
- Psychopharmacology
- Electroconvulsive therapy
- Diet, nutrition and exercise
- Individual and group psychotherapy
- Working with the family of the older adult
- Clinical psychiatry in the nursing homes
- The continuum of care: movement toward the community
- Acute care inpatient and day hospital treatment
THIRD YEAR
Related allied diagnostic and research sciences in Geriatric Mental Health with recent advances
I: Special Topics:
• Legal, ethical and policy issues
• Integrated community services and rehabilitation
• Housing for elderly
• Yoga/meditation and its applications in mental health.
• The past and future of Geriatric Psychiatry
• Generational conflicts
II: Recent Advances:
• Basic Sciences: Neuroanatomy, Neurophysiology, Neuropathology, and Neuro-psychopharmacology
• Applied Sciences: Phenomenology, diagnosis, management, rehabilitation
• Other Special Issues: Forensic Geriatric Mental Health, Liaison Geriatric Mental Health and Community Geriatric Mental Health.
III: Methods of Clinical Research:
• Descriptive Statistics
- Univariate: central tendency, skewness and Kurtosis
- Bivariate: regression and correlation Coefficient
- Special measure of association: Rank Order Correlation Coefficient, Tetrachonic Correlation Coefficient and Phi – Coefficient.
• Probability
- Probability laws, Binominal, Poisson and normal distributions, sampling from finite population, sample size, sample spare, Student t- statistics, Chi-square statistics, F-Variate, statistical inference.
- Estimation, point estimation, interval estimation, test of hypothesis, Type I and Type II errors, tests based on student-t, Chi-Square, V- Variate, proportion tests, tests of goodness of Fit: 2 x 2 contingency table, 2 x r contingency table, r x c contingency table.
• Analysis of Variance:
- Basic models, assumptions, One way and Two-way classifications, Analysis of covariance Multiple variate analysis: principle component analysis, Factor analysis, Cluster analysis, Discriminate function analysis, Multiple Regression, Data processing and Computer analysis.
• Non-parametric Statistics:
- Central limit theorem, One sample and Two sample problems, Analysis of variance of rank order statistics.
• Scientific Method:
- Procedures to ascertain knowledge, scientific method and its features, Courses and effect: Mill’s canons.
• Theory of Measurement:
- Measurement Nominal, Ordinal, Interval and Constructing Rating scales and Attitude Scales, Validity Ratio Scales, Reliability scale.
• Epidemiological Studies:
- Prospective and retrospective studies, prevalence, incidence, age- specific disease and adjusted rates, Life Table technique.
• Survey Technique:
- Various tools, Mail Questionnaire and interview schedule
- Sampling Methods: complete enumeration, sample survey, sampling and non-sampling errors, random and non-random samples
- Sample Random, Systematic Random, Stratified Random and Cluster Random Sampling Design; methods of minimizing non-sampling errors.
• Experimental Design:
- Experiments versus Surveys, general principles in experimental design, requirements for a good design, methods of controlling experimental errors, idea of control, matching, local control, concomitant variation, randomization and replication.
- Completely randomized design, randomized block design, Latin Square design, Factorial designs and Cross-Over design.
TEACHING AND LEARNING METHODS
Teaching methodology
1. This should include regular case presentations, didactic lectures, seminars, journal clubs, clinical meetings, and combined conferences with allied departments. The post graduate student should be given the responsibility of managing and caring for patients in a gradual manner under supervision. Lectures are to be kept to a minimum. They may, however, be employed for teaching certain topics. Lectures may be didactic or integrated. Didactic lectures are of least importance.
2. Department should encourage e-learning activities.
3. Formal teaching sessions
In addition to bedside teaching rounds, at least 5-hr of formal teaching per week are necessary. The departments may select a mix of activities as given under formative assessment.
The students should also attend:
• accredited scientific meetings (CME, symposia, and conferences).
• additional sessions on basic sciences, biostatistics, research methodology, teaching methodology, hospital waste management, health economics, medical ethics and legal issues related to medical practice.
4. There should be a training program on Research methodology to build capacity to guide research.
5. The post graduate student shall be required to participate in the teaching and training program of undergraduate students and interns.
6. A post graduate student of a postgraduate degree course in broad specialties/super specialties would be required to present one poster presentation, to read one paper at a national/state conference and to present one research paper which should be published/accepted for publication/sent for publication during the period of his postgraduate studies so as to make him eligible to appear at the post graduate degree examination.
7. Log book: During the training period, the post graduate student should maintain a Log Book indicating the duration of the postings/work done. This should indicate the procedures assisted and performed, and the teaching sessions attended. The Log book shall be checked and assessed periodically by the faculty members imparting the training.
8. Research work
Research Project & publication: Every post graduate student shall carry out research work on assigned research project under the guidance of a Post Graduate teacher, the result of which shall be written up and submitted for publication.
9. Journal Club: 1 hour duration – Paper presentation/discussion – once per week.
10. Seminar: One seminar every week of one hour duration (afternoon)
11. Lecture/discussion: Lectures on newer topics by faculty, in place of seminar as per need.
12. Case presentation in the ward and the afternoon special clinic (both long case and short case). Post graduate students will present a clinical case for discussion before a faculty and discussion made pertaining to its management and decision to be recorded in case files.
13. Case conference: Post graduate students are expected to work up one long case and three short cases and present the same to a faculty member and discuss the management.
14. Combined Round/Grand Round: These exercises are to be done once a week or twice a month involving presentation of unusual or difficult cases. Presentation of cases in clinical combined / grand rounds and clinical series/research data is for the benefit of all clinicians and other related disciplines once in a week or fortnightly. Emergency situation: Casualty duty to be arranged by rotation among the post graduate students with a faculty cover daily by rotation.
15. Bedside clinical training for patient care management. Daily for ½ to one hour during ward round with faculty and 1-2 hours in the evening by senior resident/faculty on emergency duty, bed side patient care discussions are to be made.
16. Clinical teaching: In OPD, ward rounds, apart from scheduled post graduate activities.
17. Post Graduate students shall be required to participate in the teaching and training program of Undergraduate students and interns.
18. A post graduate student of a postgraduate degree course in broad specialities/super specialities would be required to present one poster presentation, to read one paper at a national/state conference and to present one research paper which should be published/accepted for publication/sent for publication during the period of his postgraduate studies so as to make him eligible to appear at the post graduate degree examination.
19. Log books shall be maintained regularly and should be checked and assessed periodically by the faculty members imparting the training.
20. Department should encourage e-learning activities.
Clinical postings: Recommended schedule for three years training
Three years of posting as per schedule below:
1. Primarily in the Department of Geriatric Mental Health
2. A total of 26 weeks of postings in related/allied subjects, as follows:
- 8 weeks in the Department of Medicine – during first year of training
- 3 weeks in the Department of Radiodiagnosis – during first year of training
- 6 weeks in the Department of Neurology – during second year of training
- 4 weeks in the Department of Cardiology-during second year of training
- 5 weeks in the units such as Clinical Epidemiology/Biostatics and/or Community Medicine-during third year of training
During the training programme, patient safety is of paramount importance; therefore, skills are to be learnt initially on the models / skill labs (affective / psychomotor) later to be performed under supervision followed by performing independently. For this purpose, provision of skills laboratories in medical colleges is mandatory.
ASSESSMENT
FORMATIVE ASSESSMENT during the training includes:
Formative assessment should be continual and should assess medical knowledge, patient care, procedural & academic skills, interpersonal skills, professionalism, self-directed learning and ability to practice in the system.
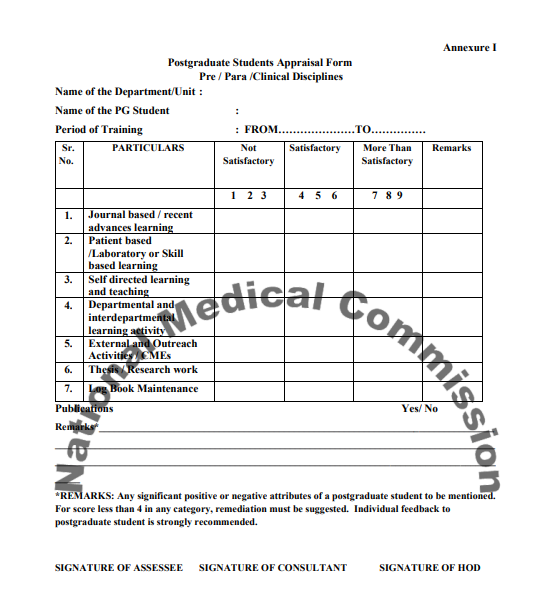
Quarterly assessment during the DM training should be based on:
1. Journal based / recent advances learning
2. Patient based /Laboratory or Skill based learning
3. Self directed learning and teaching
4. Departmental and interdepartmental learning activity
5. External and Outreach Activities / CMEs
The student is to be assessed periodically as per categories listed in postgraduate student appraisal form (Annexure I).
SUMMATIVE ASSESSMENT, at the end of training:
The Post Graduate examination for DM shall be in two parts: –
1. Theory Examination: There shall be four theory papers as follows:
Paper I: Basic Sciences in Geriatric Mental Health
Paper II: Principles and Practice of applied sciences (clinical) in Geriatric Mental Health
Paper III: Allied diagnostic and research sciences in Geriatric Mental Health
Paper IV: Recent advances in Geriatric Mental Health
2. Clinical and Practical: The practical examination should consist of the following: Clinical examination for the candidates in Geriatric Mental Health shall be conducted to test the knowledge and competence of the candidates for undertaking independent work as a specialist/teacher, for which candidates shall examine with a minimum one long case and two short cases.
The Practical examination for DM students in Geriatric Mental Health shall be conducted to test the knowledge and competence of the students for making valid and relevant observation based on the experimental/laboratory studies and his/her ability to perform such studies as are relevant to his/her subject.
The clinical examination consists of the following activities
a) One long case (Geriatric Mental Health)
b) Two short cases (one Psychiatry & one Neurology)
c) Spots consisting of EEG, Neuro-imaging and psychological testing instruments
d) Oral examination
3. Viva-voce Examination
The oral examination shall be through and shall aim at assessing the student’s knowledge and competence about the subject, investigative procedures, therapeutic techniques and other aspects of the Geriatric Mental Health which form a part of examination.
Recommended Books and Journals Text books (recent edition)
Psychiatry
1. Allan I.F Scott (eds). The ECT Hand book, The Royal College of Psychiatrists
2. Gabbard, G, Beck, JS and Holmes J. Oxford textbook of Psychotherapy, Oxford, Oxford University Press.
3. Gelder M, Andreasen N, Lopez-Ibor J, and Geddes J. (eds). The new Oxford text book of Psychiatry, Oxford University Press, Oxford.
4. Johnstone EC. Freeman C, Zealley A (eds). Companion to Psychiatric studies, Edinburgh; Churchill Livingstone.
5. Lishman, W.A. Organic Psychiatry; The psychological consequences of cerebral disorder, Blackwell, Oxford.
6. Levenson, J.L. The American Psychiatric Publishing Text book of Psychosomatic medicine, American Psychiatric publishing Inc. Washington DC.
7. Lowinson JH, Ruiz p, Hillman RB, Langrod JG (eds). Substance abuse; A Comprehensive text book, Baltimore MD, Williams & Wilkins.
8. Michels R et al (eds). Psychiatry, JB Lippencott Philadelphia, 182.
9. Ministry of Health and Family Welfare. National Mental Health Programme Booklet DGHS. New Delhi, 1982
10. Hales RE,.Yudofsky SC, Talbott, JA (eds). Text book of Psychiatry, JPB Publishers New Delhi.
11. Slater E. Roth M, Mayer-Gross, Slater and Roth’s Clinical Psychiatry, Bailliere – Tindall, London, UK.
12. Stoudemire A, Fogel BS (eds). Psychiatric care of the medical patient Oxford University press, New York.
13. Taylor, D, Paton C, Kerwin D. The Maudsley Prescribing Guidelines. Taylor and Francis, London.
14. Thornicroft, Gand Szmukler, G. Text book of Community Psychiatry, Oxford University Press, Oxford.
15. Tasman, Kay and Lieberman (eds). Psychiatry, Wiley.
16. Vyas JN, Ahuja N. (eds). Text book of Postgraduate Psychiatry, JPB Publishes New Delhi.
17. World Health Organization. The ICD 10 classification of mental and behavioral disorders, clinical descriptions and diagnostic guidelines, World Health Organization, Geneva.
18. Yudofsky SC, Hales RD (eds). Text book of Neuropsychiatry, Washington DC, American Psychiatric Press.
Neurology
1. Ropper AH and Brown RH. Adams and Victor’s Principles of Neurology, McGraw – Hill.
2. Bradley, Walter G, Neurology in Clinical Practice, Elsevier.
3. John Philp Patten. Neurological differential diagnosis Springer – Verlag London Ltd.
4. Spillane J. Bickerstaff’s Neurological examination in clinical practice Blackwell Science.
5. Mazzoni P, Lewis P. Rowland. Merritt’s neurology Handbook. Lippencott.
6. Wadia NH. Neurological practice: An Indian Perspective, Elsevier.
7. Pincus J, Tucker GJ. Behavioural Neurology. Oxford University Press, Newyark.
8. William W Campbell. Dejong’s The Neurologic Examination. Lippincott Williams & Wilkins.
Psychology
1. Clifford T. Morgan, Introduction to Psychology, McGraw Hill.
2. Smith EE, Susan Nolen – Hveksenma, Fredrickson B, Akinson G & Hilgard introduction to Psychology. Wadsworth publishing.
3. Irwin G. Savason Abnormal Psychology; The problem of Mal-adaptive behavior. Prentice Hall.
4. John W. McDavid & Herbert Haravi. Social psychology individual, groups, societies Harper & Row Publishers, Inc, US 183.
5. Robert S, Feldman. Understanding psychology. McGraw Hill.
6. Baron RA. Psychology, Allyn & Bacon.
7. American Text book of geriatric psychiatry.
Journals
03-05 international Journals and 02 national (all indexed) journals