AUSTRALIA: According to research reported in Stroke, retinal age gap was substantially linked with arterial stiffness index and incident CVD events, confirming the usefulness of this novel biomarker in predicting individuals who are at risk of future CVD events.
Globally, the main factor contributing to morbidity and mortality is cardiovascular disease (CVD). Reducing CVD morbidity and death requires prevention and early detection. As a result, numerous CVD risk calculators have been devised. However, the inaccuracy, information bias for questionnaire-based models, and the need for invasive procedures restrict the accuracy of these risk prediction models.
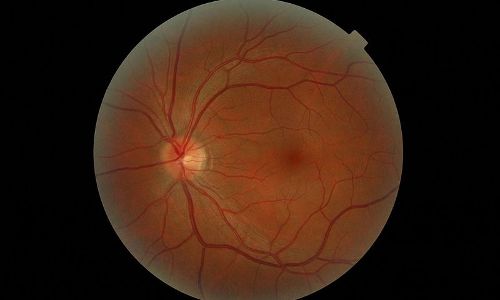
Retinal characteristics may represent circulatory alterations throughout the body. The researchers have developed an algorithm to estimate retinal age based on fundus images, which could be a potential biomarker for aging and mortality due to advancements in deep learning technology.
Therefore, the study sought to explore links between the retinal age gap, arterial stiffness index, and the occurrence of cardiovascular disease (CVD).
To estimate the retinal age, a deep learning model was developed using 19,200 fundus pictures from 11,052 participants with no prior medical history. For the other 35,917 participants, the retinal age gap (retinal age projected minus chronological age) was calculated. The relationship between the retinal age gap and the arterial stiffness index was evaluated using regression models. The relationship between the retinal age gap and incident CVD was investigated using Cox proportional hazards regression models and constrained cubic splines.
Conclusive points of the trial:
- Increased vascular stiffness index was linked to every 1-year rise in retinal age gap (β=0.002 [95% CI, 0.001-0.003]; P<0.001).
- A CVD was developed in 675 people (2.00%) after a median follow-up of 5.83 years (interquartile range: 5.73-5.97).
- In the fully adjusted model, the incidence of incident CVD increased by 3% for every 1-year increase in retinal age difference (hazard ratio=1.03 [95% CI, 1.01-1.06]; P=0.014).
- When the retinal age gap reached 1.21, according to the restricted cubic splines analysis, the risk of incident CVD considerably increased (hazard ratio=1.05 [95% CI, 1.00-1.10]; P-overall 0.0001; P-nonlinear 0.0681).
The researchers came to the conclusion that a DLA-induced retinal age difference was positively correlated with ASI and CVD incidence risk in the future.
This study provided evidence that a novel biomarker for assessing CVD risk, spotting it early, and keeping an eye on it could be the retinal age gap.
“To validate our findings across various populations, additional research is required,” they added.
REFERENCE
Zhu Z, Chen Y, Wang W, Wang Y, Hu W, Shang X, Liao H, Shi D, Huang Y, Ha J, Tan Z, Kiburg KV, Zhang X, Tang S, Yu H, Yang X, He M. Association of Retinal Age Gap With Arterial Stiffness and Incident Cardiovascular Disease. Stroke. 2022 Nov;53(11):3320-3328. doi: 10.1161/STROKEAHA.122.038809. Epub 2022 Jul 26. PMID: 35880520.
