“Never doubt that a small group of thoughtful, committed citizens can change the world; indeed, it’s the only thing that ever has,” had said the famous anthropologist, Margaret Mead. Imbibing these values, a small group of people in India and Philippines have changed the lives of many people affected by tuberculosis (TB) – especially those who were being missed or left behind by public services. TB, despite being preventable and curable, continues to be the deadliest of infectious diseases in high TB burden countries. In 2023 TB infected 10.8 million people and killed 1.25 million people worldwide.
Globally almost a third of people who get active TB disease every year are missed. The number of people with TB who are missed in high burden settings (almost all in the Global South) is alarmingly higher than the global average.
More worryingly, we also miss TB among those who take a TB test. Almost half of those who get a TB test worldwide, are tested through sputum microscopy – an outdated test that underperforms and is likely to miss finding TB in around half of those who take this test. But when we see the numbers in high burden settings, use of underperforming microscopy is higher. For example, in India – a country with highest TB burden worldwide – as per India TB Report 2024, 79% of TB tests in 2023 were done using the underperforming microscopy (which misses around half of them). That is why the World Health Organization (WHO) had called upon in 2018 to replace all microscopy with upfront molecular testing by 2027.
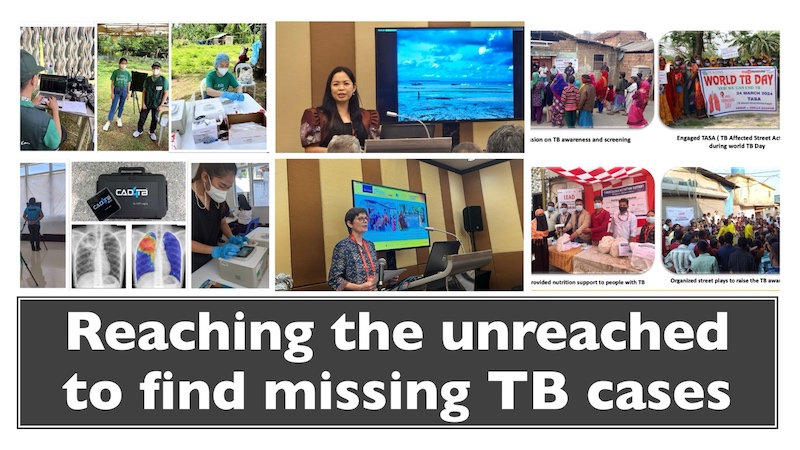
Selfless doctor on a #HealthForAll mission in Philippines
In multiple islets of Bantayan in the northernmost part of Cebu, Philippines, only around one-third of the estimated TB cases could be notified before the pandemic. But after the introduction of new TB screening and diagnostic tools, now almost all the TB (99%) is found in 2024.
Bantayan has 25 barangays (small townships) and one district hospital which is understaffed and undersupplied. These areas are also marked as geographically isolated and disadvantaged areas (GIDA). Pump boats are the main form of transportation here. Most of the residents there are fisherfolk or farmers and their income is a humble 300-350 Pesos (USD 6-7) a day.
Using latest and state-of-the-art TB screening and diagnostic tools in the Philippines was made possible in 2022 through the Introducing New Tools Project (iNTP) of the Stop TB Partnership, United States Agency for International Development (USAID) and FHI360. These new diagnostic tools included computer and artificial intelligence aided ultraportable handheld X-ray machines of Fujifilm (to screen for TB) and point-of-care, laboratory independent and decentralised WHO-recommended molecular test Truenat of Molbio Diagnostics (to diagnose TB). Both, Truenat and ultraportable X-ray machines, are battery operated, and can be deployed at point of need, even in remote and hard to reach areas like the Bantayan islets.
When these new tools were deployed in Bantayan islets, new TB case notifications, as well as treatment success rate, increased manifold. But the journey was not easy.
Braving inclement weather and carrying these new innovative diagnostic tools for TB in moulded plastic tubs, Dr Samantha Tinsay, the Municipal Health Officer of Bantayan, leads her team from islet to islet on pump boats, to screen and diagnose people with TB. She was speaking at a session in the world’s largest TB and lung disease conference this year (Union World Conference on Lung Health in Indonesia 2024).
Her untiring efforts have resulted in a tremendous increase in TB case finding: the number of persons screened for presumptive TB went up from 187 (in 2019) to 2506 (in 2022), 2027 (in 2023), and 5679 people in 2024. The target for presumptive TB screening for 2024 was set at 2248 people, but Dr Samantha’s team has already screened 253% more than the target this year.
Before the pandemic, 187 people with active TB diseases were found (39% of the estimated cases). After introduction of new TB screening and diagnostic tools, Dr Samantha’s team found 458 people with TB in 2022, 341 in 2023 and 394 in 2024 so far. Before the pandemic, 39% of estimated TB cases were found but after introduction of new tools, 99% of estimated TB cases are found by Dr Samantha and team.
All people found with TB were linked to TB treatment on the same day.
“TB treatment success rate has also increased to 97% in 2023,” she confirmed. Average TB treatment success rate in the Philippines was 78% in 2023 as per the WHO Global TB Report 2024.
Imagine the difference it can make in the Philippines’ response to end TB if such interventions can be scaled up and become a norm.
As per the latest WHO Global TB Report 2024, out of the estimated 739,000 people with TB in the Philippines, around 77% (575,800) were notified to the national programme, and over 37,000 lives were lost due to TB in 2023. Also, only 65% of those reached, got a WHO recommended molecular test diagnosis.
“When the going gets tough, the tough gets going”
When Dr Samantha Tinsay embarked on her journey to find TB with new tools in September 2022, extreme climate events- such as typhoons and storms- compounded the challenge. But it was sheer determination on her and her team’s part to hop on a pump boat and brave the storms and typhoons to go from islet to islet and find TB, treat TB and prevent TB.
The X-ray and Truenat molecular test were brought to the Bantayan Rural Health Unit and packed in a suitcase with wheels for transportation. Both these machines fitted well in a moulded plastic tub and were transported via pump boats.
On 29 October 2022, Tropical Storm Nalgae, locally known as Paeng, hit the Philippines, and affected around 4.8 million people within a week. On that fateful day, Dr Samantha Tinsay and her team were enroute to one of the islets with the diagnostics tools in tow. “As we were out of the range of mobile signal, we did not know that a storm signal had been raised, and that nobody should be travelling or working. Nevertheless, rain or sunshine, we were working and could not have stopped as patients were already waiting for us at the clinic,” said the spirited Tinsay.
Integrated healthcare
“We bundle a lot other health services, and not just focus on TB”, says Dr Samantha. Her team delivers a range of healthcare services when they go from islet to islet, such as HIV testing, hepatitis testing, dental, laboratory and diagnostics, psychiatric, psychological and mental healthcare services, among others. Those with TB, HIV or hepatitis, are linked to treatment care and support on the same day. Dr Samantha is also leveraging technology, an example of which is the setting up of a Starlink (a satellite constellation system that provides satellite-based internet service) in the middle of a basketball court.
In recognition of her efforts to strengthen local health systems, Municipality of Bantayan received three Awards- (i) Excellence in Newborn Screening, (ii) Andres Bonifacio Award, and (iii) Nominee, Best in Local Health Systems- in November 2024.
Making a difference where it is needed most: Reaching the homeless and migrant people with TB services
CNS team has met and listened to the intense journeys of almost a 100 homeless people, unauthorised slum dwellers, and migrants who could only access TB services (and get cured) because of a novel initiative implemented by Humana People to People India. Despite living in the proximity of the best of TB and healthcare facilities in major metropolitan cities of India, homeless and migrant people often slip on the blindspot.
Poor and congested living conditions, alcoholism, tobacco smoking, stigma and comorbidities (such as malnutrition and chronic lung diseases) increase their TB risk.
Lisbeth Aarup, Programme Head, Humana People to People India said that her team developed a model called LEAD (Leveraging, Engaging, Advocating for Disruption of TB transmission). Its first phase was implemented in 2023-2024 in 4 cities of India: Delhi, Hyderabad, Howrah and peri-urban Mumbai. LEAD was supported by USAID, JSI India, and Government of India’s National TB Elimination Programme.
Lisbeth’s team at Humana had trained several frontline healthcare workers (mostly women) who worked with a range of experts to help support homeless people and migrants access existing public healthcare services (as well as some private or non-profit healthcare facilities, for instance for x-rays, nutrition support, etc). Lisbeth was speaking at a session at Union World Conference on Lung Health 2024 in Indonesia.
Humana helped those most in need (and most likely to be left behind) to access health and social support services with dignity and rights.
Standard quality TB screening and diagnostics, treatments, care and support became accessible to those who could not even get a TB test earlier. Diagnostic delays and catastrophic costs often go in tandem and get more pronounced in marginalised populations.
Humana’s entire team deserves a salute for their dedication in ensuring that a person is supported in every possible way in his/ her/ their journey from TB diagnosis to cure. With those CNS could speak to, a lot of them (after completing their treatment) were actively involved as TB survivors, championing the cause of helping support the drive to raise awareness, dispel myths and misconceptions, find more TB, and help support them through the treatment. No wonder ‘lost- to- follow up’ (when people drop off from care and are unable to complete treatment) was almost negligible. This stands out because of two reasons: one, none of them would have been reached with TB services sans approaches on line with Humana model, and second, risk of left to follow up would have been probably the highest amongst them! Thank you Humana.
Humana’s team also leveraged upon new technologies, such as artificial intelligence aided cough sound-based TB screening app, as well an upfront x-ray to screen those with presumptive TB.
“During the last year we have reached out to more than 150,000 people,” said Lisbeth Aarup of Humana. “We should test the people who do not have symptoms because in the slums where we have many homeless people and migrants, we find people with TB too late. We should have found them long before!”
Lisbeth is right: if we find people with TB when they are asymptomatic and link them to effective treatment, we can stop the spread of pulmonary TB. Breaking the chain of transmission is key if we are to end TB.
Learning from experience, Lisbeth’s team goes to the people when they are more likely to be available (early morning, evening or night).
Along with LEAD, Humana People to People India is also implementing Project SWEET (Street Women Empowered and Engaged to Stop TB) that is focussed on reaching and engaging female homeless people and migrants with quality TB services, with support of Stop TB Partnership.
About 25-30% of people tested for TB (as part of LEAD’s first phase) could get an upfront molecular test in public services so far. 100% of those who get a TB test should get upfront molecular test. This is necessary if we are to stop missing TB cases.
As early and accurate TB diagnosis is the gateway to TB care pathway (and breaking the chain of infection transmission), all of us must ensure that:
* All TB services are people-centred, human rights-based and gender transformative
* We screen everyone in high burden settings (regardless of TB symptoms) with WHO recommended TB screening tools
* All those who are screened as presumptive TB cases should get upfront molecular test, and be linked to effective treatment, care and support – preferably on the same day
* TB programmes must integrate other healthcare and social support services too as needed and appropriate (for example, nutrition, shelter, quitting tobacco and alcohol, HIV and hepatitis test and treatment, NCDs, among others)
* We must reach out to those who are likely to be on the blindspot of routine public services in a sustained manner, with models such as those developed by Humana.
Initiatives led by Lisbeth and Samantha and their team are sterling examples that change is possible despite obstacles. Would governments scale these initiatives up at mass level?
