Monkeypox lesions: What do we know so far?
Tue, 09/20/2022 – 13:41
DynaMed editorial team
The rash associated with monkeypox goes through several stages. Read about and see images of the progression of lesions during monkeypox infection.

Last updated on Aug. 30
You have likely heard about the current monkeypox outbreak, which has been identified in 89 countries, 82 of which have not historically reported any cases of monkeypox. The World Health Organization (WHO) has declared monkeypox a global health emergency, with cases continuing to rise worldwide. Before the 2022 outbreak, monkeypox had been reported mostly in Central and West Africa, with almost all cases reported outside of Africa being related to international travel or imported animals from endemic regions.
Monkeypox is a viral disease related to smallpox. While symptoms include fever, fatigue and myalgia, one of the most common symptoms of monkeypox is a rash, which often resembles the rashes associated with herpes, chancroid and varicella zoster (shingles). This rash may be located in the genital or perianal areas, as well as the hands, feet, chest and face (including in the mouth). Most people develop 10-150 lesions, though it’s not unheard of for a person to develop as few as one lesion or up to 200. Interestingly, the rash is behaving differently in the current outbreak and may not appear across many parts of the body as it has with other outbreaks. Rather, it may be localized to the genital or perianal area.
The monkeypox rash goes through multiple stages and can initially look like pimples or blisters and may be itchy or painful. It is often the pain that leads a person to seek treatment. The timeline of lesion development varies: the first lesions typically appear in the genital or perianal areas but also may appear on hands, feet, chest or face. Macular lesions (flat, nonpalpable) appear over one to two days. Then, the lesions become papular (raised) for another couple days, followed by another one to two days of a vesicular rash, when the lesions are raised and filled with clear fluid. The next stage of lesion development lasts five to seven days, when pustules (raised, deep-seated, filled with opaque fluid) form. These lesions usually have a depression in the center and are usually round. Finally, the pustules start to scab over and take one to two weeks to fall off.
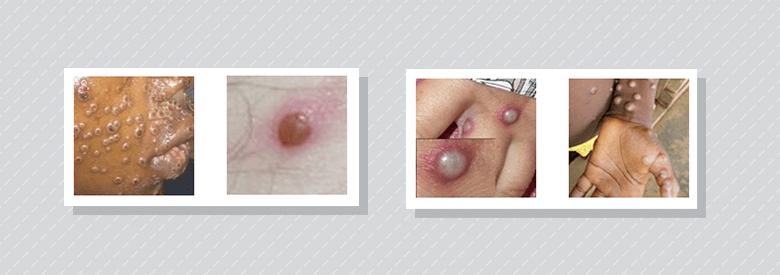
Characteristics of monkeypox skin findings: Umbilicated pustules on the face and lips, some with central crusting (far left); vesicopustule with erythematous base (second from left); pustules with erythematous base (second from right); pustules on the anterior wrist, palm and abdomen (far right). Image courtesy of Centers for Disease Control and Prevention. Reference to specific commercial products, manufacturers, companies, or trademarks does not constitute its endorsement or recommendation by the U.S. Government, Department of Health and Human Services, or Centers for Disease Control and Prevention. This material is otherwise available on the CDC website for no charge: Clinical Recognition | Monkeypox | Poxvirus | CDC
Monkeypox symptoms usually appear within three weeks of exposure and if the person develops a fever, they will likely develop the rash one to four days later. Most people have monkeypox for two to four weeks and as long as the person still has lesions, they are considered contagious.
Since monkeypox can resemble rashes associated with several other conditions, one challenge is narrowing the differential. The patterns of spread and progression of lesions contain clues. One distinctive feature about the rash associated with monkeypox is the evolution of the lesions – macular to papular, vesicular to pustular, and finally, scabbing. If monkeypox is suspected, a polymerase chain reaction (PCR) test can be performed.

Umbilicated pustules on the forehead, some with crusting (left). Hands of an individual with monkeypox in the recuperative period exhibiting eroded vesicles in same stage of healing (right). Copyright statement: Image courtesy of DermNet NZ (right), Image courtesy of CDC/Science Photo Library (left).
With the 2022 outbreak, many cases involve lesions that are localized to the genital and/or perianal areas, which has caused some confusion with common sexually transmitted infections (STIs). Monkeypox should be considered whenever a patient appears with a rash in these areas, especially if they have traveled to an endemic area, have had close contact with someone with a similar looking rash, and/or is a man who has sex with men. While the 2022 outbreak is spreading primarily among gay men, it is notable that it is not restricted to this population and monkeypox should be considered in anyone (including children) with the characteristic rash.
Medical therapy with tecovirimat is available for persons with monkeypox with severe disease including hemorrhagic disease, confluent lesions, sepsis, encephalitis, requiring hospitalization or with lesions in mucocutaneous sites which may constitute a special hazard such as eyes, mouth, genitals or anus.
If a person has been vaccinated against smallpox, research shows that they are at lower risk of developing monkeypox, as the smallpox vaccine is about 85% effective in preventing monkeypox. However, many people under age 50 have not received the smallpox vaccine since vaccination stopped being routinely administered in Canada and the United States in 1972, with the last naturally occurring case diagnosed in 1977. The World Health Assembly announced that smallpox was completely eradicated in 1980.
Even though monkeypox is spreading, it is still considered quite rare, with fewer than 50,000 cases worldwide as of Aug. 30, 2022. However, if a person suspects they have monkeypox, they should take measures to prevent the spread of the virus (staying away from people and animals, and not sharing anything that they have touched with others) and contact their health care provider.
Related posts
Five things you need to know about monkeypox
See DynaMed’s open-access Monkeypox summary
Original article, written by Lucia Kubik, MSN, RN, and published in EBM Focus
CMA members have access to DynaMed, a point-of-care reference tool valued at US$399 per year, as part of their membership.
Do you have a question on monkeypox or another clinical topic? Contact the Ask a Librarian team to request a literature search.
About the author(s)
DynaMed is a clinician-focused tool designed to facilitate efficient and evidence-based patient care. Rigorous, daily review of medical literature by physician and specialist staff ensures timely and objective analysis, synthesis and guidance. DynaMed includes drug content from Micromedex, Canadian and international guidelines, and clinical images. CMA members have access to DynaMed, a point-of-care tool, included with their membership ― a tool valued at US$399 a year.
monkeypox-lesions-what-do-we-know-so-far

