
Food allergy is an emerging health issue in our country. It is an adverse effect arising from
a specific immune response occurring on exposure to a particular food. Food allergy must
be differentiated from food intolerance, which is general nonspecific term for any adverse
reaction to particular constituent of food.
Cow’s milk protein allergy (CMPA) is the most common food allergy in infancy, with
reported prevalence of 1.5–3% in infancy and fall to <1% by 6 years of age.
Cow's milk protein allergy is more likelihood of affecting children with other atopic
conditions such as asthma, allergic rhinitis, and eczema among others, or with a family
background of allergies. About 10–15% of children who have CMPA are also allergic to soy.
The Indian
Academy of Pediatrics (IAP) has released Standard Treatment Guidelines 2022 for
Cow’s Milk Protein Allergy in Children. The
lead author for these guidelines Cow’s Milk Protein Allergy in Children is Dr. RK Gupta along
with co-author Dr. Soumya Nagarajan and Dr. Dhanesh Volvekar. The guidelines come Under the Auspices of the IAP Action
Plan 2022, and the members of the IAP Standard Treatment Guidelines Committee
include Chairperson Remesh Kumar R, IAP Coordinator Vineet Saxena, National Coordinators SS
Kamath, Vinod H Ratageri, Member Secretaries Krishna Mohan R, Vishnu Mohan PT
and Members Santanu Deb, Surender Singh Bisht, Prashant Kariya, Narmada Ashok,
Pawan Kalyan.
are the major recommendations of guidelines:
attributed incorrectly to many symptoms.
recognized, timely recognition of non-IgE-mediated CMPA can be a diagnostic dilemma,
due to delayed onset of presentation and overlapping with functional gastrointestinal (GI)
disorders.
non-IgE-mediated or mixed type CMPA, symptoms occur after 2 hours up to 2 days or
even 1 week
|
TABLE 1: Symptoms and signs of CMPA. |
||
|
IgE-mediated symptoms |
Non-IgE-mediated symptoms |
|
|
Skin |
Urticaria, angioedema, and rashes |
Acute flaring of atopic dermatitis |
|
Respiratory |
Wheezing, cough, running nose, conjunctivitis, and laryngeal edema |
Heiner syndrome (a rare form of pulmonary hemosiderosis) |
|
Gastrointestinal |
Vomiting, GERD, |
Fresh bleeding per rectum, watery diarrhea, failure to thrive, protein losing enteropathy, occult gastrointestinal bleeding, reflux |
|
Cardiovascular |
Hypotension and tachycardia |
Iron deficiency anemia |
|
Systemic |
Anaphylaxis |
Failure to thrive |
syndrome (FPIES), and food protein-induced proctocolitis (FPIP) are distinct clinical entities
associated with non-IgE-mediated CMPA.
to protein transfer via breast milk with symptoms of blood and mucus streaking
in otherwise normal stools. This settles within 48–72 hours of cow’s milk protein
elimination from mother’s diet and generally resolves by 1 year of age.
food allergies, lactose intolerance, immunodeficiency, infectious enterocolitis, irritable bowel
syndrome, Meckel’s diverticulum, cystic fibrosis, pancreatic insufficiency, etc.
Lactose intolerance is commonly confused with CMPA, presents with loose stool and
flatulence but without vomiting, blood in stool or any other system involvement (Table 2). Most
common variety is secondary lactose intolerance due to loss of brush border lactase expression
secondary to inflammation or structural damage, usually gastroenteritis. Usually resolves by
2 weeks exclusion of lactase in diet. Primary and congenital variety is rare and permanent.
|
TABLE 2: Differences between |
||
|
CMPA |
Lactose intolerance |
|
|
Types |
IgE and non-IgE-mediated |
Due to deficiency of lactase |
|
Mechanism |
It is an immune-mediated reaction |
Quantity-dependent so small amount |
|
Symptoms |
Multisystem involvement (GIT, |
Only gastrointestinal (diarrhea, flatulence, and pain) |
|
Natural history |
Recovers by 4–5 years of age in majority of people |
Recovers in days/weeks in secondary, permanent in congenital and primary types |
E)
is pathognomonic of the condition. Clinical clues that suggest IgE-mediated disease are the
involvement of two or more systems, commonly the skin, GI, and respiratory tract. On the
contrary, non-IgE-mediated disease (which is more common in India) may manifest with only
GI symptoms.
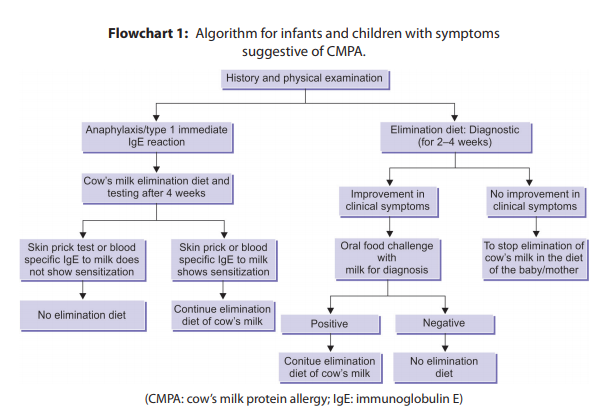
In cases where IgE-mediated variety is suspected, skin prick testing (SPT) and/or blood test
for specific IgE can be considered. When non-IgE-mediated case is suspected, elimination of
milk protein from diet and oral challenge after improvements in clinical symptoms confirms
the diagnosis (Flowchart 1).
cautiously in the following manner: 1 mL, 3 mL, 10 mL, 30 mL, and 100 mL (given
every 30 minutes), which can be done on an outpatient basis. The child should be
observed for 2 hours, and then sent home with an instruction to continue at least
200 mL of milk/day and to stop if there is recurrence of symptoms. The child should
be reviewed after 2 weeks.
administered in hospital setup in more graded fashion (0.1 mL, 0.3 mL, 1 mL, 3 mL, 10 mL,
30 mL, and 100 mL: given every 30 minutes) as an inpatient with all resuscitation
facilities including injection adrenaline to manage anaphylaxis. A positive reaction
to milk introduction confirms the diagnosis of CMPA. If no reactions occur, 200
mL/day of milk is continued for 2 weeks to look for any delayed manifestations.
Placebo-controlled
Food Challenge:
are time consuming and expensive. Endoscopy/histopathology will be of help
in unexplained cases only.
IgE levels. As of now, atopic patch test is not recommended by any standard
guidelines. Basophil histamine release assay and lymphocyte stimulation are
used in research setup. Component resolved diagnosis (CRD) or molecular level
antigen testing should not be used in routine.
Source:Indian Academy of Pediatric Guidelines
Treatment:
Strict avoidance of CMP for a defined period and reintroduction at right time is the key
to management. Early and accurate diagnosis is important, as delayed diagnosis may
result in failure to thrive and anemia while overdiagnosis results in unnecessary dietary
restrictions and economic burden.
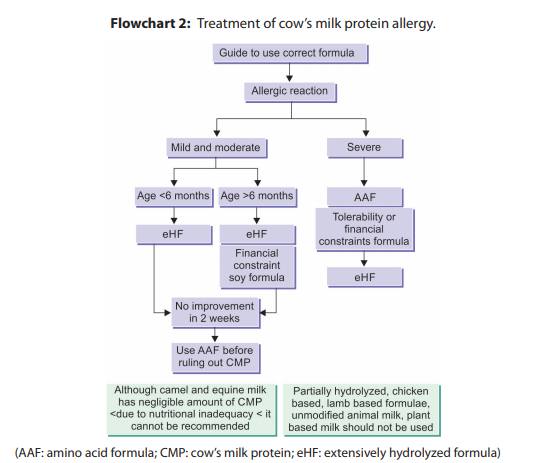
diet). Elimination diets are usually started with extensively hydrolyzed formula (eHF), with
improvement in about 90% of children with CMPA. Amino acid formula (AAF) is used in
severe CMPA or when child is not responding to eHF even after 14 days. Elimination diet
should be continued for at least 1 year and reevaluation done every 6 months.
these as a substitute is not likely to improve symptoms.
10% of affected infants react to soy protein, with higher proportions in infants younger
than 6 months so not to be used in <6 months age.
epinephrine (1:1,000) should be used immediately. Patients with anaphylaxis need to be
evaluated and monitored in an emergency room, even if the symptoms improve with
epinephrine. This is because there is a risk of a “second wave” of symptoms occurring after
the epinephrine wears off.
incidence of CMPA is lower (0.5%) in exclusively breastfed infants compared to formula-fed or
mixed-fed infants.
allergy can come up in 50% and to inhalants by 50–80% before puberty.
- Caffarelli C, Baldi F, Bendandi B, Calzone L, Marani M, Pasquinelli P. Cow’s milk protein allergy in
Further Reading
children: a practical guide. Ital J Pediatr. 2010;36:5. - Koletzko S, Niggemann B, Arato A, Dias JA, Heuschkel R, Husby S, et al. Diagnostic approach and
management of cow’s-milk protein allergy in infants and children: ESPGHAN GI Committee practical
guidelines. J Pediatr Gastroenterol Nutr. 2012;55(2):221-9. - Luyt D, Ball H, Makwana N, Green MR, Bravin K, Nasser SM, et al. BSACI guideline for the diagnosis
and management of cow’s milk allergy. Clin Exp Allergy. 2014;44(5):642-72. - Matthai J, Sathiasekharan M, Poddar U, Sibal A, Srivastava A, Waikar Y, et al. Guidelines on diagnosis
and management of cow’s milk protein allergy. Indian Pediatr. 2020;57:723-9. - Vandenplas Y. Prevention and management of cow’s milk allergy in non-exclusively breastfed
infants. Nutrients. 2017;9(7):731.
The guidelines can be accessed on the official site of IAP: https://iapindia.org/standard-treatment-guidelines/
